This story appears in VICE Magazine's Burnout and Escapism Issue. Click here to subscribe.I remember standing next to my mother and my aunt in a drab hospital waiting room in Summit, New Jersey, when the nurse delivered a diagnosis. They’d found a mass in my grandmother’s brain. It was cancerous and aggressive—a glioblastoma, they called it—so they’d have to operate. It was the same type of cancer that John McCain had. My grandmother, however, is not a white man, so her journey would inevitably be a little different.
Advertisement
My grandmother, Louise Kennedy Evans Elder, grew up in the 40s and 50s during Jim Crow in the heat of Spartanburg, South Carolina. She remembers playing with chickens in her backyard as a child. “It was what we used to do for fun,” she tells me. “We were poor, but my parents never let us know we were poor. My mother would make our clothes and my father made sure we never wanted for anything. I wish they pushed education, but my folks weren’t educated people, so they did the best they could with what they had.”There were 13 children altogether—she was number 10. When she was a small child, their home caught fire and she lost her younger siblings. From that moment on, she was referred to as the baby. When she was 13, the family moved to New Jersey, and at 15 she was pregnant with my mother, which forced her to hit adulthood before she got to high school. By 16 she was a married housewife, and at 19 she began her career in nursing.Before the glioblastoma, she’d already beaten cancer in both her lungs and in her breasts—she had her first mastectomy 34 years ago. That day, after the diagnosis, she decided to fight for her life again.Some would call the cancer streak bad luck, but those of us who understand what it means to be black in America can easily identify it as something more complex. New research and a more conscious exploration of health disparities in this country show us that black Americans have worse health outcomes than white Americans across the board. What’s more—they’ve found that even if you’re black in America with a sound bank account, you can’t buy whiteness.
Advertisement
“Weathering,” a term coined by race disparities scholar Arline Geronimus, is the deterioration of health as a result of the chronic stress of being exposed to systemic racism for your whole life—the product of an accumulation of “lifelong physiological stress-mediated wear and tear,” Geronimus said. As someone who lives it, I can say it’s like a thousand paper cuts to the body and mind, a slow and sometimes subtle degradation.Even as history books, documentaries, and museum plaques have discussed slavery on a macro level, I and other black writers are often dismissed when we link our current well-being to the trickle-down trauma of that first slave boat hitting the shore of Virginia almost exactly 400 years ago.I sometimes wonder what happens in our brains when we see the photos of the scars of our ancestors—when we see the pictures of white Americans celebrating the lynchings of our family members who hung from trees less than a hundred years ago. Is it a similar chemical reaction to when we watched the viral video of Eric Garner getting choked out by a cop on a Staten Island sidewalk?
More from Tonic:
My grandmother grew up in a time when the Klan was an active part of her daily life. She tells me about her inability to speak back to white people who disrespected her, or even make eye contact with them when walking by. To this day, my grandmother still doesn’t know who murdered her father in the barn next to their home—she only knows it was done by repeated blunt trauma to the head.
More from Tonic:

My grandmother grew up in a time when the Klan was an active part of her daily life. She tells me about her inability to speak back to white people who disrespected her, or even make eye contact with them when walking by. To this day, my grandmother still doesn’t know who murdered her father in the barn next to their home—she only knows it was done by repeated blunt trauma to the head.
Advertisement

People like me can still see and touch our ancestors who were clubbed by police, bitten by dogs, and hosed down like animals. If it seems like I’m anchored by the past, consider the rope that’s tied to that anchor—every single thing since then that’s shaped how my community gets to live, learn, eat, and access care.Consider the medical crimes committed against us—the Tuskegee study or J. Marion Sims’s experiments on slave women sans anesthesia, for example—that have planted seeds of mistrust for doctors. Consider that medical professionals often don’t believe some of us when we say we’re in pain—it’s reflected in the underdiagnosis of disease and the denial of pain medications for black Americans who actually need them.And then there is the way conditions such as HIV, because of cultural stigma and socioeconomic factors, continue to harm our communities at higher rates than they do white communities. The NAACP reminds us that while black and white Americans do drugs at similar rates, our system jails black people for it almost six times more that white people, strategically destroying a portion of America’s family structures. All these factors play a major role in how long and how well we get to live.After Jim Crow, neighborhoods in American cities were segregated so that black Americans could live in the less desirable areas. More formally, one tool to enforce this was redlining, the “systematic multisector, multilevel-of-government exclusion of African Americans, not just from the ability to buy a home but the crucial ability to accumulate wealth,” said Jason Purnell, a professor of public health at Washington University in St. Louis and the director of For the Sake of All, a health equity research initiative. “This has to be the center of any narrative for trying to understand the kinds of disparities that we see today.”
Advertisement
Where your family lives dictates everything from the quality of education you have access to, to the magnitude of daily stressors you’ll encounter, including racial micro- and macro-aggressions that serve as constant reminders that we are “the other.” For some, these stressors cut deeper, and include the unique grief of losing a loved one whom society seemed to thoughtlessly discard. Evident disparities along with these stressors can equate to a chronic toll on our health, even if there are resources within our reach.“What a lot of people probably don’t understand is that the availability of healthcare—even if it’s high quality healthcare—only accounts for 10 to 20 percent of health outcomes,” Purnell said. “So even if you had wonderful access to healthcare, which many people don’t, you still only put a small dent in things like disease and mortality.”Being rich and black won’t exempt you from social stressors, either. (Last year Serena Williams, who nearly died following the birth of her daughter, pointed to a CDC report that stated that black women in the United States are more than three times more likely to die from childbirth-related causes.) “There are ways in which being black in a more secure or affluent community causes new stressors that can weather you,” Geronimus told me. “If you’re thrust into a world that runs by the dominant cultural framework, which is the one that marginalizes you as a black person—so now you’re in some sense, being ‘othered,’ or worried about representing your race.” Having to manage your identity in these types of atmospheres takes constant vigilance, which can activate physiological stress responses.
Advertisement
A 2014 report from Purnell and his collaborators at For the Sake of All showed that a black American woman who has a college degree or more is still more likely to deliver a baby at a low birth weight than a white woman who has graduated from high school. Black women who are highly educated and making good money “are dealing with the stress of interacting—probably at a greater frequency—with people outside of their racial group,” Purnell told me.The way in which race has weathered us is overwhelming, but it does not define us. It is, however, something that the healthcare system has continued to deny for centuries. And when it’s not denied, it’s conveniently attributed solely to class.“People think well, if we solve poverty, then we will have solved problems of race,” Purnell said. “But there’s still significant stigma associated with African American identity, no matter how successful you are.”Other times the paper cuts are not so subtle. For example, my heart races every time I see the flashing blue lights of a police car. I’m reminded that even if I abide by every rule, I could somehow end up dead in the back of one of their squad cars. There are also the constant videos trending on social media in which we see our people being abused or executed, and the internalizing of that pain chips away at our psyche a little at a time.There’s a very specific toll grief takes on the body—especially the uniqueness of loss linked to racial bias. When Eric Garner was killed by Officer Daniel Pantaleo that July afternoon in 2014, his dying words—“I can’t breathe”—became a somber mantra for millions of people.
Advertisement
“There was Pantaleo who choked him to death,” said Gwen Carr, Eric Garner’s mother, who lives in Staten Island. “There were other police officers who pounced on him. There was another police officer, who stood back and did not try to deescalate the situation, and still other officers who lied on police reports before the video came out. All of them are guilty, including the EMS.” She said that the first responders did not intervene and save her son and that they should also be held accountable for his death.Garner lost his life to the very system that’s been criminalizing, condemning—and many, including myself, would argue—enslaving black men in America with a biased justice system as its vehicle. According to CNN, 80 officers have been arrested on murder or manslaughter charges for on-duty shootings in the past decade. Only 35 percent were convicted, while the others remained either not convicted or awaiting trial. “This would happen far less if they held people accountable. They let it go on like it’s all right,” Carr said.Garner’s daughter Erica took up the fight for her father to ensure that neither his name nor his plight would ever be forgotten. She led marches, protested police brutality by lying for hours in the spot where he died, and threw herself into a life of impassioned advocacy. “Erica fought hard for her father. She wanted to seek justice,” Carr said. “She would go all over the country with different organizations. They would rally. They had grief, as she did. I think it was such a strain on her. It took such a toll.”
Advertisement
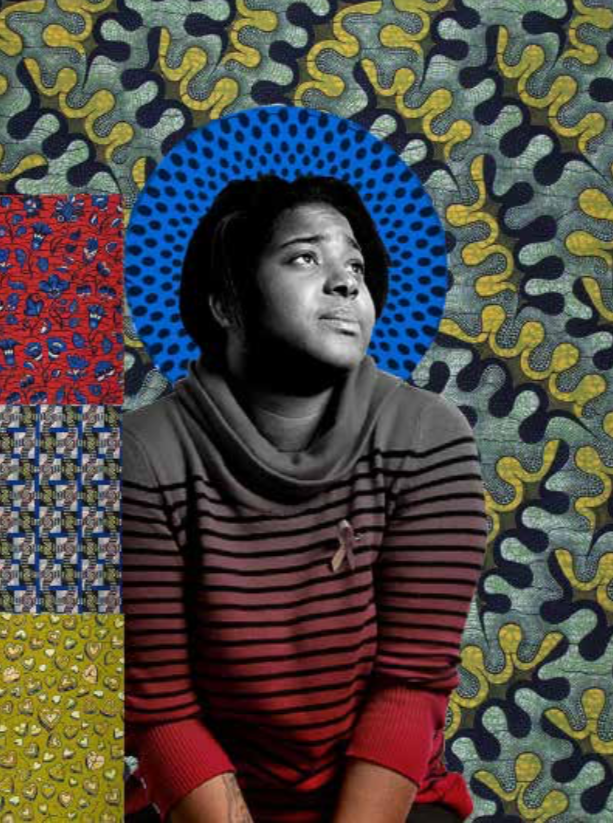
Erica Garner died in December of 2017, at 27, in a medically induced coma that doctors placed her in after she suffered brain damage from a heart attack. It was apparently her second that year. Her mother, Esaw Snipes, told the New York Times that her daughter developed heart problems earlier in 2017, after giving birth to her second child.“She never had heart problems that I knew of before,” Carr said. “The strain of her having the baby, the strain of her loss of her father, and strain she put on herself by lashing out at everybody—there was all of that too.”Erica’s death following her father’s so closely is not a tragic coincidence. Geronimus points to the weathering-related vulnerabilities she faced. “And then you have the incredible stress of losing her father in the way she lost him. The video is everywhere. I don’t think there’s any surprise here, but people do dismiss it as ‘she already had a heart problem.’”Venida Browder’s death 16 months after her son, Kalief, killed himself—after spending nearly two years in solitary confinement at Rikers Island after being indicted (but not convicted) for theft—that’s not a coincidence either. The deterioration of health that permeates an entire family unit is tied to that anchor that won’t shift until we see it for what it is: Racism is robbing black Americans of decades of their lives.In younger black people there are increasing rates of suicide, twice the rate of white children. I myself am black, queer, and living with HIV—a virus the CDC tells me will infect 50 percent of black men who have sex with men over their lifetime. My generation has watched the executions of Tamir Rice, Renisha McBride, Jordan Davis, and Trayvon Martin—who were all under the age of 25—by either police or regular citizens who took it upon themselves to play racist cop.
Advertisement
My grandmother survived her surgery, but this will likely be her final one. Doctors have told us all they can do now is a monthly chemo treatment to keep the tumors at bay, but in many cases they return. Most people live only about a year following surgery. I wonder, out loud with her, what it’s like to fight cancer most of your adult life and win multiple times, only to have it appear in a place where it’s nearly impossible to fight. “It’s well with my soul,” she tells me. “I don’t have any regrets. I had a good life. The only thing that bothers me is that I’m leaving my children and grandchildren, and that hurts. But I know they will be fine, ’cause I raised them all to be great people. I’m all right. My family will be all right.”Despite how anti-black this world has been to my grandmother and to so many people who look like her, she’s found reasons to find joy in the worst conditions—it’s a skill that runs through her blood as well as mine. We have always been resilient against a world that continues to treat us as less than fully human.What awaits her when she gets home is something else that she may be unable to afford: The new level of care she’ll require will become our responsibility—an additional layer of stress for everyone involved, although we won’t let it show.
I see evidence of what race scholars and health researchers have been saying about looking to the past for acts of self-preservation to adopt in order to shift health outcomes. “Not to say we want to go back to segregation, but there were self-help behaviors that segregation necessitated,” said Alfiee Breland-Noble, a psychologist and mental health disparities researcher at Georgetown University’s Center for Trauma and the Community. “You couldn’t go to the doctor by yourself because you didn’t know what was going to happen. Someone always needed to be waiting in the lobby for you just in case.”She says even today, someone should be in the lobby waiting. We need to physically be there for each other, advocate for each other, and vocally set a standard of care. Take notes, ask questions, and make sure the physician is listening to you or your family member, Breland-Noble says. “The physician or the psychologist or social worker—they’re an expert in their field. But you are an expert in your body.”And even when you’re not in the hospital, having time set aside every week to spend time with people who look like you and who carry similar burdens and joys, can slow the damage of weathering. Purnell says that being around people of a similar ethnic background can be “protective, from a mental health standpoint,” against internalizing discrimination, isolation, and anxiety. I liken it to the euphoria I experience every time I go back to my HBCU (historically black college or university) homecoming or family reunion.It all seems kind of wholesome—leaning on your community as a cure-all of sorts. I continue to grapple with the idea that race’s effect on health is less about access and more about identity than I thought. It’s a disconcerting thought, when you’re living with wounds that never seem to be given the time or space to ever properly heal.Sign up for our newsletter to get the best of Tonic delivered to your inbox.