Stocktrek Images/Getty Images
Melinda Gates recently declared that the biggest threat to humanity is a pandemic brought on by a bioterrorist attack. The scenario evokes a horror movie complete with villains, mysterious laboratories, and global devastation. But before scenes from Contagion start flashing through your mind, it’s worth investigating what an outbreak would actually look like and how concerned experts really are about the possibility of an attack.The top contenders for biological weapons are classified as Category A agents by the Centers for Disease Control and Prevention (CDC). The top threats are anthrax, botulism, plague, smallpox, tularemia, and viral hemorrhagic fevers, such as Ebola, Dengue, and Marburg.No matter what agent is deployed, a few key attributes determine how deadly an outbreak will be. A pathogen becomes more dangerous when it can be grown in large quantities, stay intact longer, exist in smaller particles, require a lower dose to infect people, spread easily, and lead more infected people to develop an illness.The overarching threat of bioterrorism is that a bad actor or nation would increase those attributes for one of the Category A agents, says Mark Kortepeter, a professor of epidemiology at the University of Nebraska Medical Center College of Public Health and former scientist at the US Army Medical Research Institute of Infectious Diseases. Targeting those properties is more feasible now than it was in the past, because genetic technologies make it easier and less expensive to manipulate an organism’s genome.But enhancing a pathogen is still extremely challenging. “A well-funded organization with scientific expertise and the resources to grow, manipulate, or release agents, and the motivation to actually use them—that’s the worst case scenario,” he says.Others agree that biological weapons pose a serious threat, but that significant hurdles lower the likelihood of an attack. “It’s certainly possible. But it’s hard to do. It takes a lot of money and organization and scientific expertise,” says Stephen Morse, a professor of epidemiology at the Columbia University Medical Center.Although experts seem to place the risk slightly lower than Gates, they note that serious incidents have occurred and biodefense is critical. If a bioterrorist attack were to occur, what would it look like? Let’s take a look at a hypothetical timeline of a weaponized virus.Acquisition
A person or organization, let’s call them John Doe, first has to acquire the virus. Doe could somehow gain access to stores of biological weapons that nations have already developed. For example, two secure stores of smallpox exist (one in the US and one in Russia) that experts have long debated whether to maintain or eliminate. Doe could also order a virus from a culture collection, a repository of biological material for scientists, or he could find it in nature, by seeking out animals that are susceptible to particular infections.Delivery
For a large scale attack, Doe would disseminate the virus with an aerosol device, says William Dowling, a program officer in the Office of Biodefense Research Resources and Translational Research at the NIH. Smallpox is one virus stable enough for this delivery method.Doe could also infect himself with the virus, target others to infect, or attempt to contaminate the food or water supply. But poisoning the food or water supply would be difficult, because we have strong protective measures in place, says Oliver Grundman, a clinical associate professor at the College of Pharmacy at the University of Florida.Spread
Exit John Doe, enter mother nature. A virus’s natural power to spread is what makes it so dangerous. Influenza is especially concerning, since it races through communities at startling speeds, Kortepeter says. “It’s so efficient in how it spreads. It’s like you light the kindling and then see this conflagration of a huge fire.”The speed also depends on how many people are initially infected. If 100 people are infected with smallpox, and each of them spreads the disease to three people, the outbreak could produce 4,200 cases in one year, according to simulation by the CDC. (Smallpox historically has a death rate of 30 to 40 percent but the US is stockpiling 2 million doses of a new smallpox drug called Arestvyr.)Viruses spread slower in sparse areas and faster in dense areas like schools or offices. As the world becomes increasingly interconnected, it raises our collective susceptibility. “We have worldwide air travel, increased use of public transportation, and centralization of our food supply. So if you’re trying to get a lot of people sick, we have more vulnerabilities as a society,” Morse says.
More from VICE: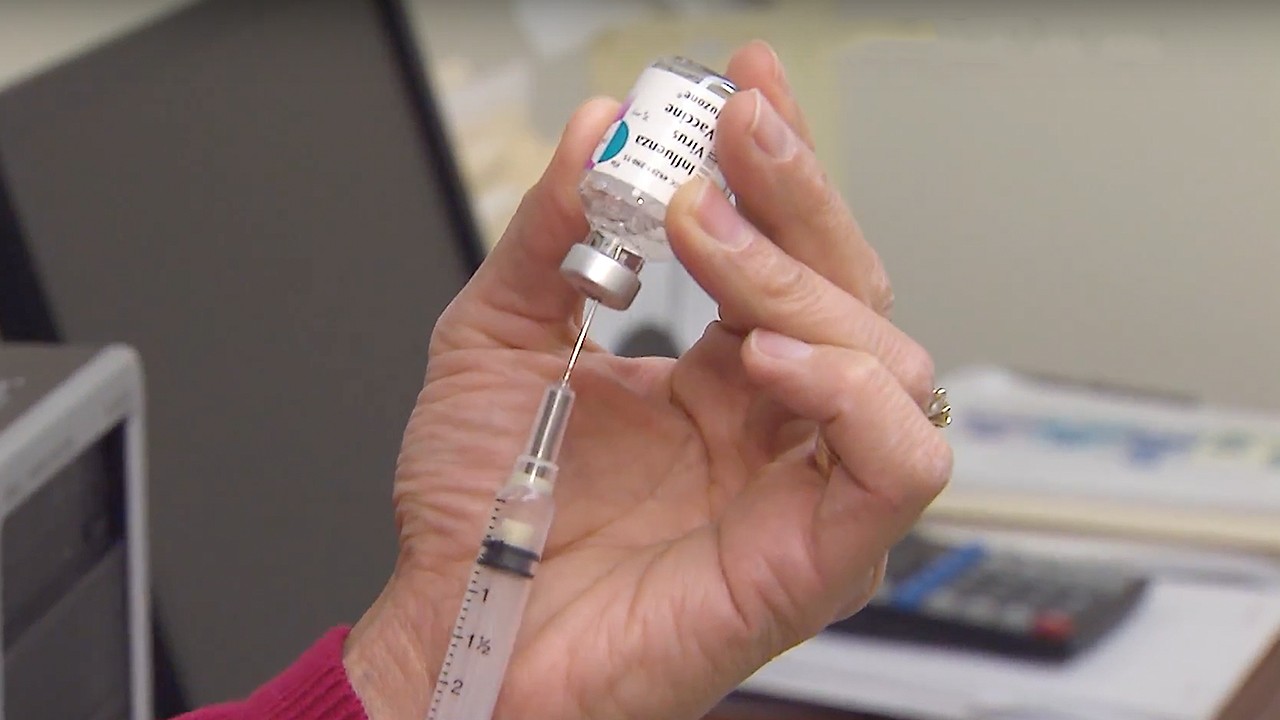
Response
When an outbreak occurs, health providers usually contact the county or city health department, which will begin investigating the situation. Based on the size and complexity of the outbreak, it might rise to the state or federal level. If the event is determined to be terrorism, the FBI will launch an investigation.Recognition
A key step in the response process is recognizing whether the outbreak was natural or intentional. That can be tricky, because a patient’s symptoms can mimic symptoms of other illnesses, and because it can take time for similar cases to materialize. “Most of these diseases start out looking exactly the same, and they look the same as 100 other diseases,” Dowling says. Public health officials will assess the number of cases, check if patients respond to normal treatments, search for multiple simultaneous outbreaks, and note whether the disease is expected in the region. Basically, everything boils down to context. “How many cases does it take to call it an epidemic? It depends on the disease. If it’s flu, it could be thousands of cases. But anthrax in the United States? One case,” Kortepeter says. Context clues provide insight, but the only definitive proof of malicious intent is physical evidence like a spray device, a letter containing anthrax spores, or a cultured organism.Containment
The medical community identifies symptoms of the disease—like a rash, fever, or paralysis—to develop a case definition. They assess how many patients fit the case definition and try to determine a diagnosis. Then they identify risk factors like who a patient came in contact with and how the disease spreads. They treat those who are ill and target those who are at risk with a vaccine or medication. They may block off certain areas or quarantine infected patients.In the CDC’s smallpox simulation, the health department uses vaccines and isolation to quell the outbreak. If they quarantine 25 percent of infected patients and if vaccination reduces the transmission rate by 33 percent, the outbreak would be contained in one year. And these are conservative estimates, so the outbreak would probably be contained sooner, says lead author Martin Meltzer, leader of the Health Economics and Modeling Unit at the CDC. “A release of smallpox is a nasty thing to contemplate. But with existing tools—the vaccine, isolation, and public health intervention—we can expect that, if we plan and prepare, we can stop that outbreak,” he says.The public health community will continue to assess and adapt their strategy throughout the response process. For example, there was a global campaign to eradicate smallpox in the late 1960s. The first strategy was to vaccinate as many people as possible around the world. But the supply soon depleted and outbreaks began popping up in communities with high vaccination rates. So in Nigeria, the team adopted a different approach. They identified which village had smallpox and vaccinated everyone in that village. Then they expanded outward in concentric circles, to eliminate the spread. The strategy worked, and it’s now known as ring vaccination. “That’s how they shut down the spread of the virus, and eventually eliminated it from the world,” Kortepeter says.Those are the key steps in how a virus might spread through society. Bioterrorism poses a serious risk for which the country must continue to research and prepare, but perhaps more dangerous and more likely are the outbreaks that sprout organically. The natural world has unleashed epidemics like Sars, Zika, Ebola, and the Spanish flu, which killed millions of people exactly 100 years ago. “At least 50 million people died, and almost half of the entire world’s population was infected. The 1918 flu was arguably the greatest natural disaster in human history,” Morse says.The public health world also struggles to correctly predict outbreaks, tending to prepare for the most recent disease rather than the one that later emerges,” Kortepeter says. “To some degree, mother nature is the most efficient bioterrorist. She’s always keeping us humble.”
Advertisement
Advertisement
A person or organization, let’s call them John Doe, first has to acquire the virus. Doe could somehow gain access to stores of biological weapons that nations have already developed. For example, two secure stores of smallpox exist (one in the US and one in Russia) that experts have long debated whether to maintain or eliminate. Doe could also order a virus from a culture collection, a repository of biological material for scientists, or he could find it in nature, by seeking out animals that are susceptible to particular infections.Delivery
For a large scale attack, Doe would disseminate the virus with an aerosol device, says William Dowling, a program officer in the Office of Biodefense Research Resources and Translational Research at the NIH. Smallpox is one virus stable enough for this delivery method.Doe could also infect himself with the virus, target others to infect, or attempt to contaminate the food or water supply. But poisoning the food or water supply would be difficult, because we have strong protective measures in place, says Oliver Grundman, a clinical associate professor at the College of Pharmacy at the University of Florida.
Advertisement
Exit John Doe, enter mother nature. A virus’s natural power to spread is what makes it so dangerous. Influenza is especially concerning, since it races through communities at startling speeds, Kortepeter says. “It’s so efficient in how it spreads. It’s like you light the kindling and then see this conflagration of a huge fire.”The speed also depends on how many people are initially infected. If 100 people are infected with smallpox, and each of them spreads the disease to three people, the outbreak could produce 4,200 cases in one year, according to simulation by the CDC. (Smallpox historically has a death rate of 30 to 40 percent but the US is stockpiling 2 million doses of a new smallpox drug called Arestvyr.)Viruses spread slower in sparse areas and faster in dense areas like schools or offices. As the world becomes increasingly interconnected, it raises our collective susceptibility. “We have worldwide air travel, increased use of public transportation, and centralization of our food supply. So if you’re trying to get a lot of people sick, we have more vulnerabilities as a society,” Morse says.
More from VICE:
Response
When an outbreak occurs, health providers usually contact the county or city health department, which will begin investigating the situation. Based on the size and complexity of the outbreak, it might rise to the state or federal level. If the event is determined to be terrorism, the FBI will launch an investigation.
Advertisement
A key step in the response process is recognizing whether the outbreak was natural or intentional. That can be tricky, because a patient’s symptoms can mimic symptoms of other illnesses, and because it can take time for similar cases to materialize. “Most of these diseases start out looking exactly the same, and they look the same as 100 other diseases,” Dowling says. Public health officials will assess the number of cases, check if patients respond to normal treatments, search for multiple simultaneous outbreaks, and note whether the disease is expected in the region. Basically, everything boils down to context. “How many cases does it take to call it an epidemic? It depends on the disease. If it’s flu, it could be thousands of cases. But anthrax in the United States? One case,” Kortepeter says. Context clues provide insight, but the only definitive proof of malicious intent is physical evidence like a spray device, a letter containing anthrax spores, or a cultured organism.Containment
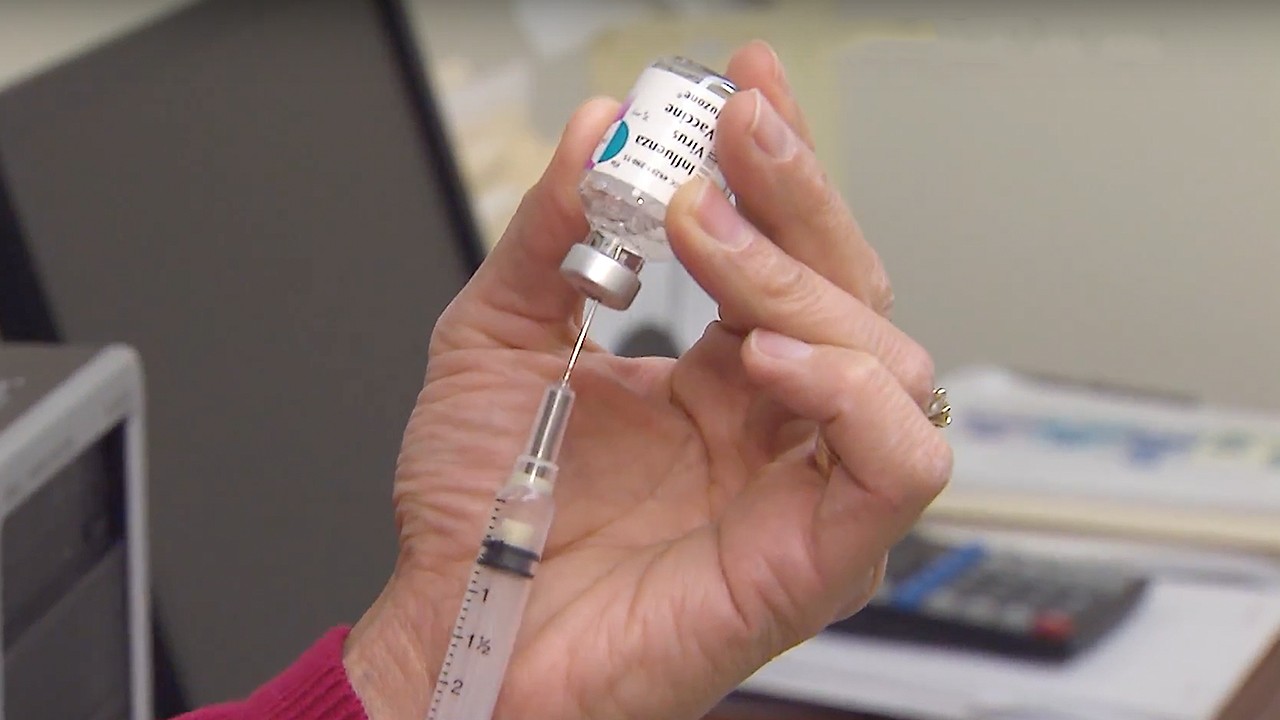
The medical community identifies symptoms of the disease—like a rash, fever, or paralysis—to develop a case definition. They assess how many patients fit the case definition and try to determine a diagnosis. Then they identify risk factors like who a patient came in contact with and how the disease spreads. They treat those who are ill and target those who are at risk with a vaccine or medication. They may block off certain areas or quarantine infected patients.
Advertisement
Advertisement
Bioterrorism also harbors a sinister motive to instill deep fear and anxiety. For instance, the anthrax letters of 2001 bred a powerful wave of terror and paralyzed the postal system. “In many cases, bioterrorist attacks are not intended to cause a whole lot of fatalities,” Grundman says. “It’s more about public anxiety. The uncertainty that it could happen anytime or anywhere causes a level of anxiety that rocks a stable society to its core.”The US has established numerous biodefense programs to combat potential attacks, such as BioWatch, BioShield, the Laboratory Response Network, and number of federal research agencies. Dowling, of the Office of Biodefense Research Resources and Translational Research, explains the agency has three research domains: diagnostics, vaccines, and therapeutics. One of the biggest pushes in the vaccine realm is to develop a universal flu vaccine. “If you had one vaccine that could cross all of the influenza viruses, or at least a good portion of them, that would make a huge impact,” Dowling says. In the other two domains, scientists are creating diagnostics and drugs to combat Ebola, Zika, Lassa, and others.Dowling agrees that a pandemic is one of society’s biggest threats, and as biotechnology becomes more accessible, the possibility of an engineered virus grows too. But as the risk of bioterrorism increases, so do our biodefense strategies. “Our tools are reacting better now,” Dowling says. “We can quickly identify a virus, get the sequence, and get some kind of countermeasure out the door pretty fast.”Sign up for our newsletter to get the best of Tonic delivered to your inbox weekly.