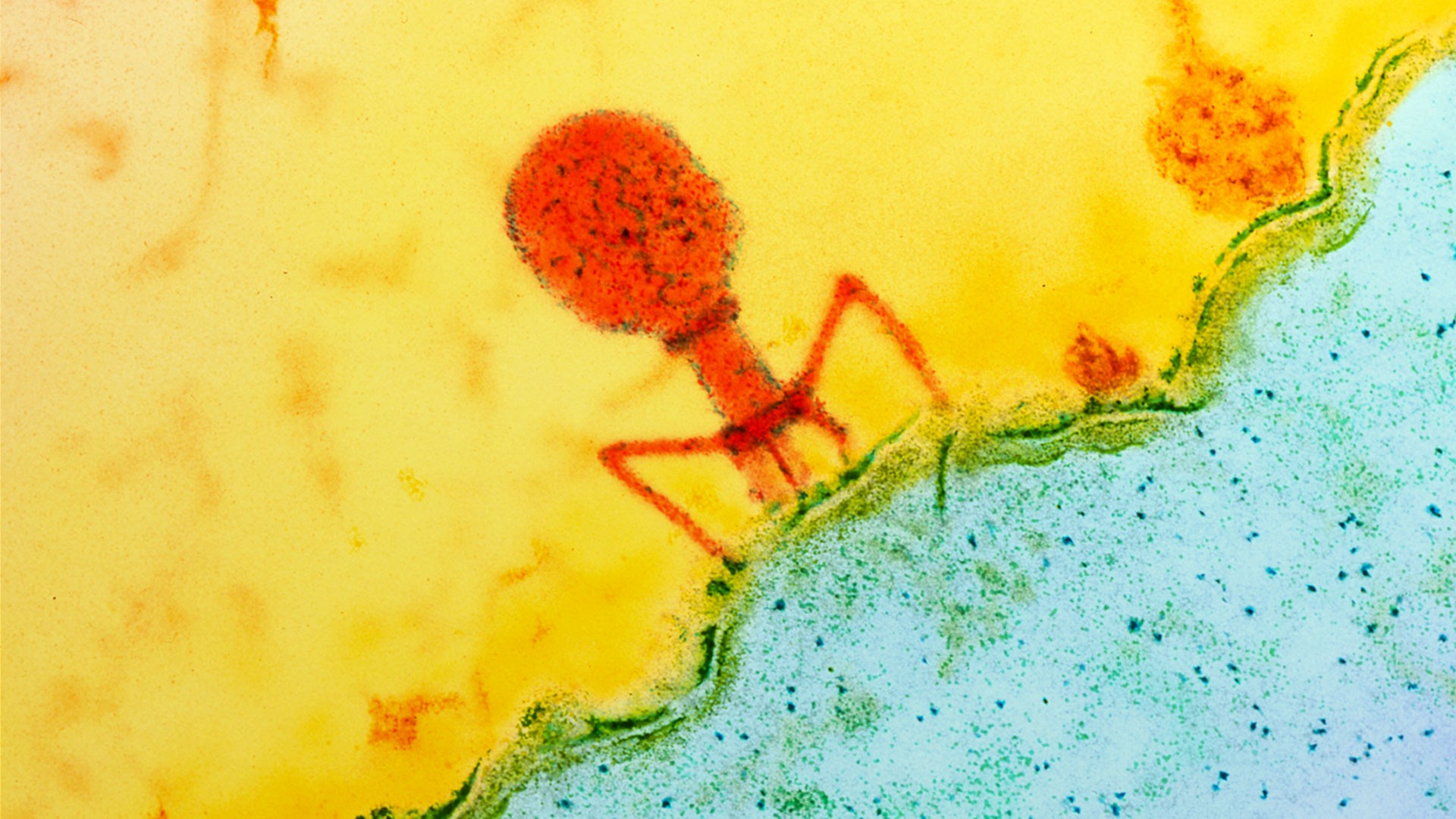
BartekSzewczyk/ Getty
On January 19, the first COVID-19 patient in the United States was diagnosed in an urgent care clinic in Snohomish County, Washington. The 35-year-old man, who had a cough and a fever, had recently visited family in Wuhan, China.He was admitted to the hospital and stable for the first few days, despite an intermittent fever. On his third day, a chest X-ray didn’t show any abnormalities. On the fifth day, that changed. His chest x-ray showed signs of pneumonia, and his ability to breathe started to deteriorate. On the sixth day the situation in his lungs was getting worse.What his doctors did next, according to their case report in the New England Journal of Medicine (NEJM), was ask for permission to give him an antiviral drug called remdesivir—which is not approved by the FDA. This is called a compassionate-use exemption, which allows very sick people to try experimental medications.They injected remdesivir on his seventh day, and by the eighth, he started getting better. He was able to go off oxygen support, and his breathing improved.It's cases like this one that have stirred hope around potential antiviral treatments for COVID-19, the illness caused by a new coronavirus SARS-CoV-2.The COVID-19 vaccine clinical trial recently enrolled their first U.S. patients, but it's going to be awhile before we're able to get it. Developing a vaccine takes time—researchers have to make sure it's safe, and do so by monitoring people for side effects over many months. Since a vaccine isn't right around the corner, antiviral and malaria drugs are now in the spotlight as a potential treatment option many countries desperately need.Remdesivir was originally tested (and proved unsuccessful) for treating Ebola. There's also the anti-malaria medications chloroquine and hydroxychloroquine, and a combination of two HIV drugs, lopinavir and ritonavir. They're all being investigated for use against COVID-19.But an unfortunate truth about medicine persists, even during a pandemic: Individual case reports, as with the man in Washington, don't necessarily mean a drug is effective and safe. While there are hundreds of clinical trials taking place around the world, researchers are saying we need to be cautious about overstating these drugs' promise until we have more information.Nonetheless, at a press conference last week, Donald Trump erroneously said that chloroquine had been approved for use for COVID-19 and that remdesivir was “essentially approved.” “They’ve gone through the approval process,” he said. “It’s been approved, and they did.”According to the FDA and CDC, however, there are no approved drugs for COVID-19. Yesterday, remdesivir received an "orphan drug" designation from the FDA, which provides certain benefits to the company, Gilead Sciences, in developing the drug, but doesn't yet make it legal.“This is a brand new disease that we've really only known about for three months or less,” said Judith James, a rheumatologist and Vice President of Clinical Affairs at the Oklahoma Medical Research Foundation.It makes sense to want a solution to appear as quickly as possible. But we still have a lot to learn.Clinical trials will help clinicians figure out key questions about these drugs. Will they work at all? At what point in the onset of the disease are they most effective? What doses should they be used in? Are there any side effects at those doses? Could they be used in combination? Could they be used to prevent COVID-19, not just treat it? We currently don’t know.Eric Rubin, a professor of immunology and infectious diseases at the Harvard T.H. Chan School of Public Health, said speculation doesn't help, data does. “All of the reliable data right now are biochemical, case reports, or short case series without controls,” he said. "We need good controlled trials.”Many of the studies that are being published are more like “experiences,” James said—meaning they’re reports of small groups or individual patients where there’s not always a control or placebo group. These early findings are critical to help guide what drugs to study more in-depth, but they're not enough to make any definitive conclusions.Last week the World Health Organization (WHO) announced that it was starting a global drug trial called SOLIDARITY. “It’s an unprecedented effort—an all-out, coordinated push to collect robust scientific data rapidly during a pandemic,” Science Magazine wrote.SOLIDARITY will be focusing on the emerging top contenders: remdesivir, chloroquine and hydroxychloroquine; lopinavir and ritonavir, along with combining lopinavir and ritonavir with interferon-beta, an immune molecule that regulates inflammation in the body.
Watch more from VICE: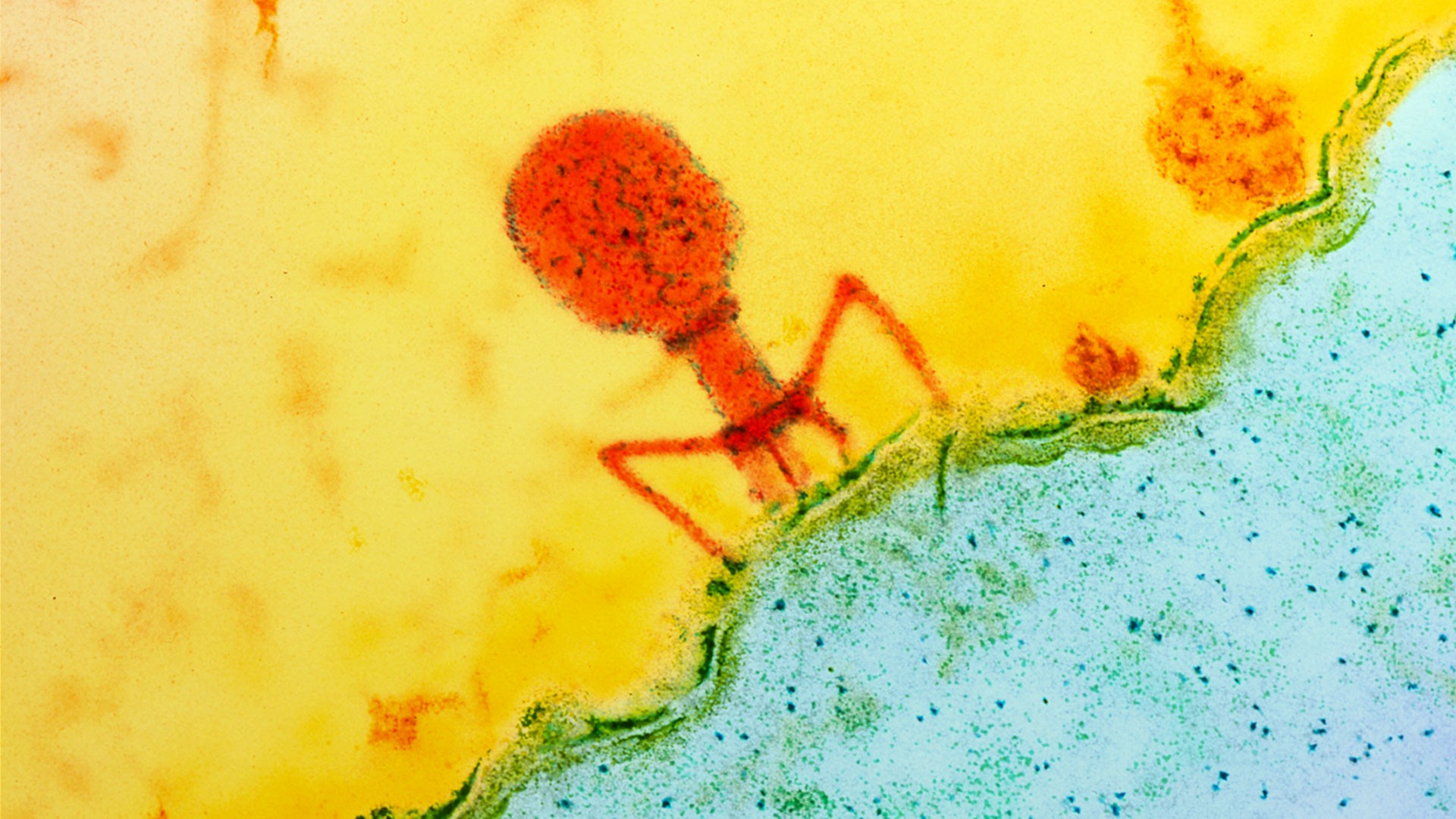
For now, the drugs are being investigated to see if they help people who are currently sick. James said that if that’s shown to work, then they will be considered if they would be helpful for prevention. Any treatment would have an impact on the course of the pandemic, especially if it decreased the rate of viral shedding and transmission, Rubin said.“But it would also have to be widely employed to make a big impact. That is certainly possible for a very safe, oral drug,” Rubin said. If a drug had risks or was only available through an injection, it would probably only be used for those who are more ill, he continued. “That could be good for folks who have severe disease but would have less of an impact on transmission.”The SOLIDARITY trial drugs had already started their journey down the drug pipeline, before COVID-19. That's a good thing: it means they would be available widely more quickly because a lot of the safety and lab experiments have already been completed.Chloroquine and a similar drug, hydroxychloroquine, for example, have already been on the market for decades. Hydroxychloroquine is used to treat rheumatoid arthritis and lupus, along with malaria. James said “if they were found to be very helpful, it would be something that we could get available to patients sooner rather than later."Chloroquine and hydroxychloroquine change the pH (or acidity levels) of cellular compartments (called endosomes and lysosomes) that viruses can hijack to take over a human cell, explained Jean Millet, a microbiologist at the Molecular Virology and Immunology unit of INRAE, located in France.Still, in New York, the U.S. state with the highest case number, governor Andrew Cuomo recently announced that they received 70,000 doses of hydroxychloroquine, 10,000 doses of azithromycin and 750,000 doses of chloroquine and that trials with these drugs will start this week.Remdesivir is an antiviral drug that has never been approved by the FDA. It acts as a kind of paper jam in the viral genome copy machine, ultimately preventing the virus from replicating. It has been shown in lab experiments to be effective against SARS and MERS—past coronaviruses, and is being tested in five clinical trials. Two of the clinical trials for remdesivir could release results as early as April.It’s important to remember that early lab results don't always replicate in humans. “When considering the development of any type of drug treatment, keep in mind that a drug that shows promise and works very well in a research laboratory does not necessarily translate into a safe and effective treatment that can be used to treat patients,” Millet said.Since SARS-Cov-2 has been shown to use its coronavirus spike to bind to human cells, it may mean that high doses of hydroxychloroquine are needed for it to interfere with the virus attaching itself to human cells. This could raise concerns about toxicity, Science reported.In Thailand, doctors reported that patients improved when they took two HIV drugs, lopinavir and ritonavir. But in 199 people with COVID-19, authors of a new paper in the NEJM wrote that people who received lopinavir–ritonavir treatment got “no benefit” from it, beyond patients who received only regular care.The authors also wrote that they had a high death rate overall—22 percent—which might have meant that their patients were especially sick, and the medicines couldn’t help when the disease was that far along. It shows how many variables there are, when considering when, how much, and which drug to give to patients.“It’s really hard to do good clinical trials whenever you're in the middle of an epidemic,” James said.Putting too much emphasis on these drugs too early could lead to other serious problems. In Arizona yesterday, a man died and his wife is in critical care after they apparently tried to self-medicate with chloroquine phosphate.After Trump's mention of chloroquine (which is available over the counter in some countries), thousands of other people have "rushed to stockpile" the drug, according to the Wall Street Journal, resulting in chloroquine and hydroxychloroquine shortages.This week, Gilead Sciences said that in response to “an exponential increase in compassionate use requests” they were no longer able to grant patients access to the drug individually, instead turning their focus to creating an expanded access program.“During this transition period, we are unable to accept new individual compassionate use requests due to an overwhelming demand over the last several days,” their statement said. They will make exceptions for pregnant women and children under 18 with confirmed and severe cases Covid-19.After some concern that the drug's "orphan drug" status, might lead the cost remdesivir to sky-rocket, Stat reported on Wednesday that Gilead asked the FDA to rescind their orphan drug designation, and is "waiving all benefits that accompany" it.For now, Millet said it’s still too early to definitively say which drug is the most promising, and how all these logistics will play out. It will take patience and perseverance to find what works best. If none of these drugs end up working, the story doesn't end there. There are almost 70 drugs and compounds that could help treat the new coronavirus, and 24 already FDA approved for other conditions, according to a preprint published on Sunday night.“We are at a point in the pandemic where I think we should be careful not to place all our hopes solely on the development of a ‘miracle drug,’” he said. The ramping up of research efforts and clinical trials are certainly encouraging and should be closely monitored. But even if a drug is proven to be safe and effective, it will be important to carefully check how the drug is being used—and for the possibility of the emergence of viral resistance to it.”Just because a drug may emerge in the next month or two doesn’t mean that we should loosen up on other measures, like social distancing, hand washing, and more.“I never want to be too negative, but I think we need to be cautiously realistic,” James said. “I think that these are options, but they’re not answers. Until we have more data, we’re not going to know. We will have a lot more data in a few months. We need to be cautiously realistic and Americans need to realize that they can’t put their hopes solely into these medications. We’re going to have to keep doing the other things we’re doing, like staying inside, and doing those better—until we get this under control.”Update 3/27/20: Information was added regarding the orphan drug status of remdesivir and new criticism about the French hydroxychloroquine preprint.Sign up for our newsletter to get the best of VICE delivered to your inbox daily.Follow Shayla Love on Twitter .
Advertisement
Remdesivir and chloroquine are promising, but they're not approved yet
Advertisement
Advertisement
How remdesivir, chloroquine, and other drugs might work against the coronavirus
Watch more from VICE:
For now, the drugs are being investigated to see if they help people who are currently sick. James said that if that’s shown to work, then they will be considered if they would be helpful for prevention. Any treatment would have an impact on the course of the pandemic, especially if it decreased the rate of viral shedding and transmission, Rubin said.“But it would also have to be widely employed to make a big impact. That is certainly possible for a very safe, oral drug,” Rubin said. If a drug had risks or was only available through an injection, it would probably only be used for those who are more ill, he continued. “That could be good for folks who have severe disease but would have less of an impact on transmission.”
Advertisement
Laboratory studies have found that chloroquine and hydroxychloroquine can stop the new coronavirus from infecting cells. In the first two weeks of March, French clinicians published a preprint on 20 patients with COVID-19 who got hydroxychloroquine along with azithromycin, an antibiotic. They reported that the people who got the drugs had a significant reduction in symptoms and that the amount of viruses in their nasal swabs went down. Since the findings were released, some scientists have questioned the validity of the data in the paper, and its overall conclusion.
Advertisement
What happens in the lab doesn't always happen in people
Advertisement
We can be optimistic, but don't hoard or take these drugs yet—or stop social distancing
Advertisement
