“Why don’t you come to my double mastectomy?” my friend Caitlin Wilterdink asked me.
It was her annual fall Friendsgiving last October; I was up to my elbows in mashed potatoes, stirring butter and salt into the creamy pot of carbs. My jaw slacked and the wooden spoon nearly fell from my hands into the sink.
Videos by VICE
“Your what?”
In August 2016, at 31, Caitlin tested positive for a mutation in her BRCA2 gene. According to Dr. Eric Mou, an Oncology Fellow Physician at Stanford Health Care, BRCA2 normally cuts down on genetic irregularities that make cells more prone to behaving abnormally. But for those who carry a mutated gene, cells can accumulate DNA damage and additional genetic mutations, which puts them at risk for having abnormal genetic function and growing into cells like those that make up cancer. According to the National Cancer Institute, approximately 45 percent of women who have the BRCA2 mutation will develop breast cancer by the time they are 70 years old.
It’s a gene Caitlin inherited from her mother, who passed away from breast cancer at 54, when Caitlin was 14. Her mother’s breast cancer was first diagnosed at 34. She had a single mastectomy at the time and went into remission, but the cancer returned in her other breast seven years later, and she battled the disease for a total of 15 years. Caitlin remembers watching her mother go through multiple surgeries and rounds of chemotherapy, knowing even at seven years old that one day she might have to do the same. Her premonition was correct: a child whose parent has a BRCA2 mutation has a 50 percent chance of receiving it.
After Caitlin’s positive test for the BRCA2 mutation, she spent the next year and a half in doctor’s appointments, mammograms, MRIs and surgeries. A 2016 mammogram revealed atypical ductal hyperplasia, an abnormal pattern of cell growth that has some features of pre-cancer and can turn into it if left untreated. Caitlin had the breast tissue containing the cells removed and it tested negative for cancer. The next year, she had a guided MRI biopsy that uncovered a second diagnosis of atypical ductal hyperplasia. She began to wonder how long this series of mammograms, MRIs, biopsies and removal would continue. That year and a half of appointments, she said, led to missing “something like two or three weeks of work,” and from everything she could see, they would only get more onerous.
At that point, her doctors told her she had three options: have another small surgery, more MRIs, and the possibility of more surgeries in the future; begin taking the drug Tamoxifen, which inhibits breast cancer growth and would likely force her body into early menopause; or have a preventative double mastectomy, removing her breasts—and the tissue that could be genetically predisposed to kill her—along with them.
At that point, she said, her breasts felt like ticking time bombs. “Let’s just do it,” she said to her doctor, and scheduled a double mastectomy with a breast reconstruction for December 11, 2017, four days after her 33rd birthday.
According to Dr. Mou, many studies clearly show that a patient who has a BRCA2 mutation can reduce their risk of developing cancer by over 90 percent with a prophylactic mastectomy. Those are good odds, and it’s not uncommon for someone around Caitlin’s age with mutations of BRCA2 and/or BRCA1 (a gene similar to BRCA2) to undergo the procedure, either: a 2010 study found that 14.7 percent of women aged 25 to 35 who were diagnosed with the mutations chose to have mastectomies.
It’s a difficult choice for women in Caitlin’s shoes: undergo an invasive surgery that will radically alter one’s relationship with their own body, with cascading effects on everything from one’s dating life and future health to the subtle, daily bodily movements most of us take for granted, or face the risks of breast cancer, an onslaught of invasive medical interventions, and possible death. As a young single woman living in New York City and a prolific marathon runner, a mastectomy might profoundly affect Caitlin’s love life, and would impact one of her great passions. But if you’re young and an invasive surgery now would greatly reduce your chance of having cancer later on, why not take it?
“I feel like doing this is a way to pay my mother back for everything she went through,” Caitlin wrote on Instagram before the procedure. “So cheers Momma, this one’s for you.”
You may have heard of BRCA before, from Angelina Jolie. In 2013, at 37 years old, the actress and director penned an op-ed for the New York Times about her decision to have a prophylactic double mastectomy after discovering she had the BRCA1 mutation that could lead to breast cancer, which caused her mother to pass away at 56.
But most people are not Angelina Jolie. It’s likely Jolie didn’t have to spend hours on the phone each time she got a medical bill like Caitlin does, first calling the doctor’s office and then the insurance company, often having to explain that yes, she is under 36 but she does qualify for insurance coverage for a mastectomy because of her high risk factors and genetic testing. Jolie also probably did not have to climb the stairs post-surgery in a fourth-floor walkup in Brooklyn, or worry about the impact of her medical procedures on her finances. Jolie may not have had to fret over the cost of taking taxis and cars while she recovered, for fear of strangers on the subway bumping into her still-healing chest, or the prospect of losing her job after having taken too many days off.

“We got here early,” Caitlin texts me. It’s 5:14 AM on December 11.
I arrive shortly thereafter. Caitlin is in the surgical patient waiting area on the 10th floor of NYU Langone’s Tisch Hospital, eyes barely open. Sitting across from her are her dad and her best friend Casey. Caitlin has had nothing to eat or drink since 8 PM last night; she’s been awake since 4 AM for a surgery scheduled at 7 AM. A nurse soon appears and whisks her behind a dark wooden door.
Not long after, we’re invited behind the door ourselves to see Caitlin before surgery. In a tiny, fluorescent-lit room, she wears a thin hospital gown and a light blue hairnet. Casey offers up a stuffed narwhal she bought, reciting ocean creature facts and the plot of Moby Dick to distract Caitlin from her surgery, now minutes away. She manages a smile and rests her head on her dad’s shoulder.

A nurse in green scrubs enters and it’s time. The room goes quiet and Caitlin leans against the doorway hugging her father. Her eyes pinch closed, small tears gently falling from each. She hugs Casey then disappears behind another dark wooden door with the nurse.
The surgical oncologist will remove the breast tissue, then the plastic surgeon will do the reconstruction with implants Caitlin picked out. She will keep her nipples, which tested negative for cancer. She’ll have stitches from the surgery and an incision in each breast will connect to a drain that will remove blood and pus, sparing her from an infection. She’ll have to empty the drains twice a day. If there is breast cancer at any point moving forward, it’ll be easily noticeable—cancer in a regular breast is more difficult to feel.
Her life as an incredibly self-sufficient and active woman is about to change drastically, and she will have to learn how to ask for help, something she told me she’s not used to doing. For a week after surgery, Caitlin will only be able to sponge-bathe herself and can’t wash her hair. She also won’t be able to run or exercise beyond walking, or lift anything heavy until she heals. It will take 4-6 weeks for her to regain her strength and escape a feeling of exhaustion.

When Caitlin’s surgery finishes, the surgical oncologist and plastic surgeon tell her father that it was a success. “She looks beautiful,” they said. They looked at the pathology of the breast tissue and, luckily, everything was clear: no cancer lurking anywhere. His eyes well up and he pulls a rumpled tissue from his pocket to wipe away unsprung tears.
When Caitlin finally reemerges, she’s lying on her back on a gurney, hooked up to all manner of machines. “I am on a lot of drugs,” she told us, smiling.

A week later, Caitlin’s drains are removed and she’s finally allowed to shower. She said that between dating and running, she’s more worried about the latter.
Caitlin’s mother had a single mastectomy the first time, and she lost her nipple. Caitlin’s father later told her that another man said he was “pretty surprised” he stuck with it, which, needless to say, infuriated him. But she knows that future partners might not all react charitably. “Some guys are probably gonna be okay with it, some are gonna be freaked out,” she said. “I don’t really know when the best time to tell people’s gonna be. I don’t really know what my comfort level with intimacy’s gonna be, whether that’s gonna change. I have to start feeling comfortable in my own skin.
“I think my biggest concern is getting myself back in running shape,” she said. And with three marathons planned for 2018, it’s easy to see why.
She’s been stretching her legs, doing arm and abdominal exercises, going for long walks, practicing deep breathing so she can exchange oxygen properly. She’ll have Paris’s marathon in April, then Berlin’s in September and Chicago’s in October. Caitlin knows it’s an ambitious goal, but she’s a headstrong woman: she already has her ideal race times in mind..
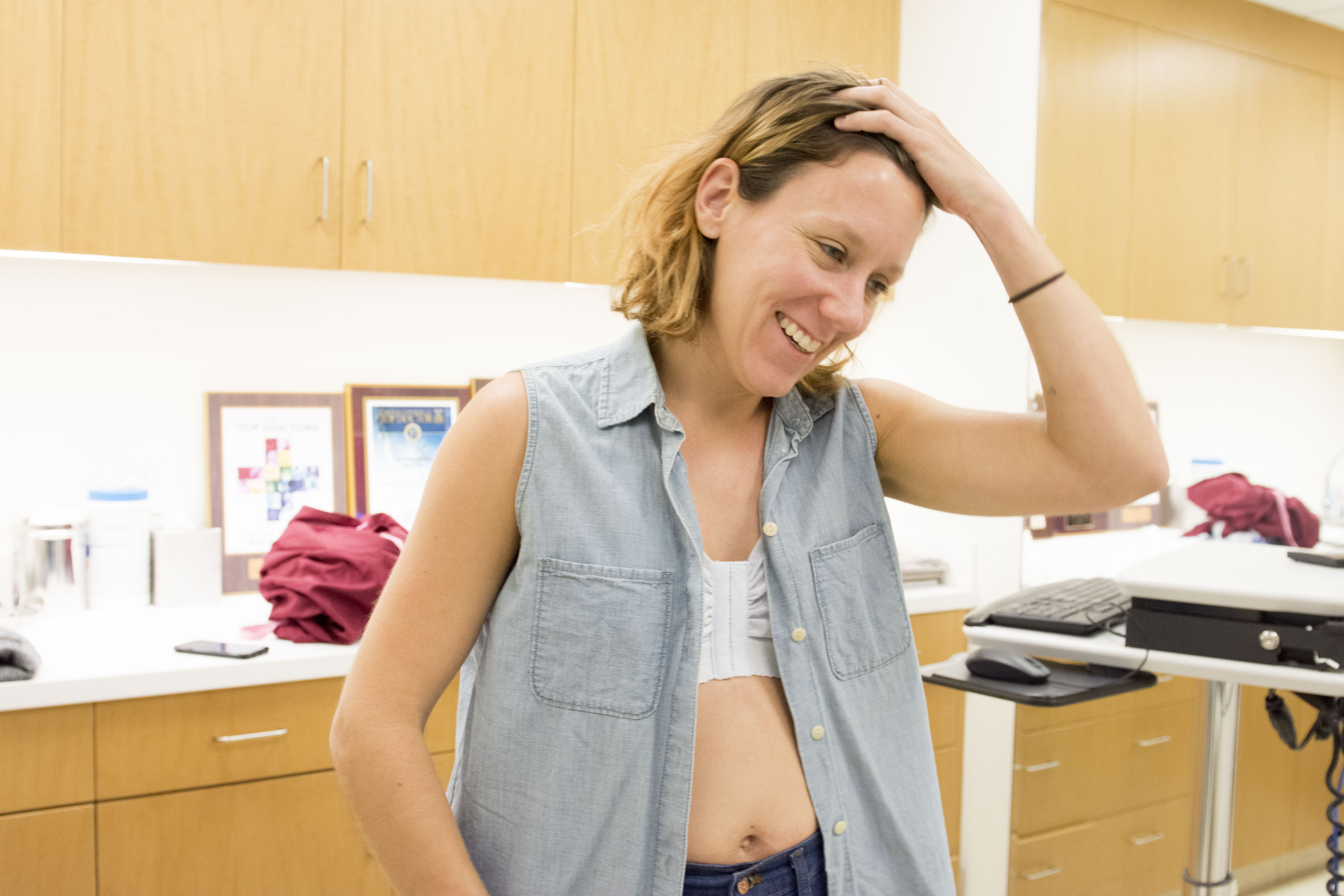
A month after her surgery, Caitlin is hosting a bar trivia night in Brooklyn. She’s dyed her hair blonde, has finally been allowed to start jogging, and is back at work. She’s doing her best to develop a sense of normalcy, but finds it frustrating that her body doesn’t yet move quite like it used to, especially when she’s running.
“This is a life-changing procedure—not only physically but also emotionally,” said Dr. Mou. Patients like Caitlin have to spend time relearning their bodies, dealing with what it means to lose a portion of themselves both literally and figuratively. Body image dissatisfaction, depression, and anxiety are real issues for recipients of mastectomies.
As Caitlin navigates her body, trains for marathons, and seeks to understand her post-mastectomy future, the hope is that the results of the surgery, while difficult to handle at the moment, will spare her the suffering her mother endured as well as the anxiety of a future with uncertain health. For now, she’s just trying to get through each day.
Dr. Mou recommends mastectomy patients like Caitlin seek support groups or counseling, but Caitlin isn’t ready for that yet. “There’s an aspect of wanting to get my life back, and that’s still in process, but there’s also unmet subconscious questions around what these feelings are actually about,” she said. “I just want to look normal and live my life.”
Follow Elyssa Goodman on Twitter.
More
From VICE
-

Photo: Beach Academy CIC / Facebook -

AEW -

Illustration by Reesa -

AEW
